Page Not Found
The page you were looking for has moved. Please contact us if you need further assistance.
For emergencies, please dial 911.
Existing Patients may visit the Patient Portal for assistance. Please allow 5 business days for response to Patient Portal requests.
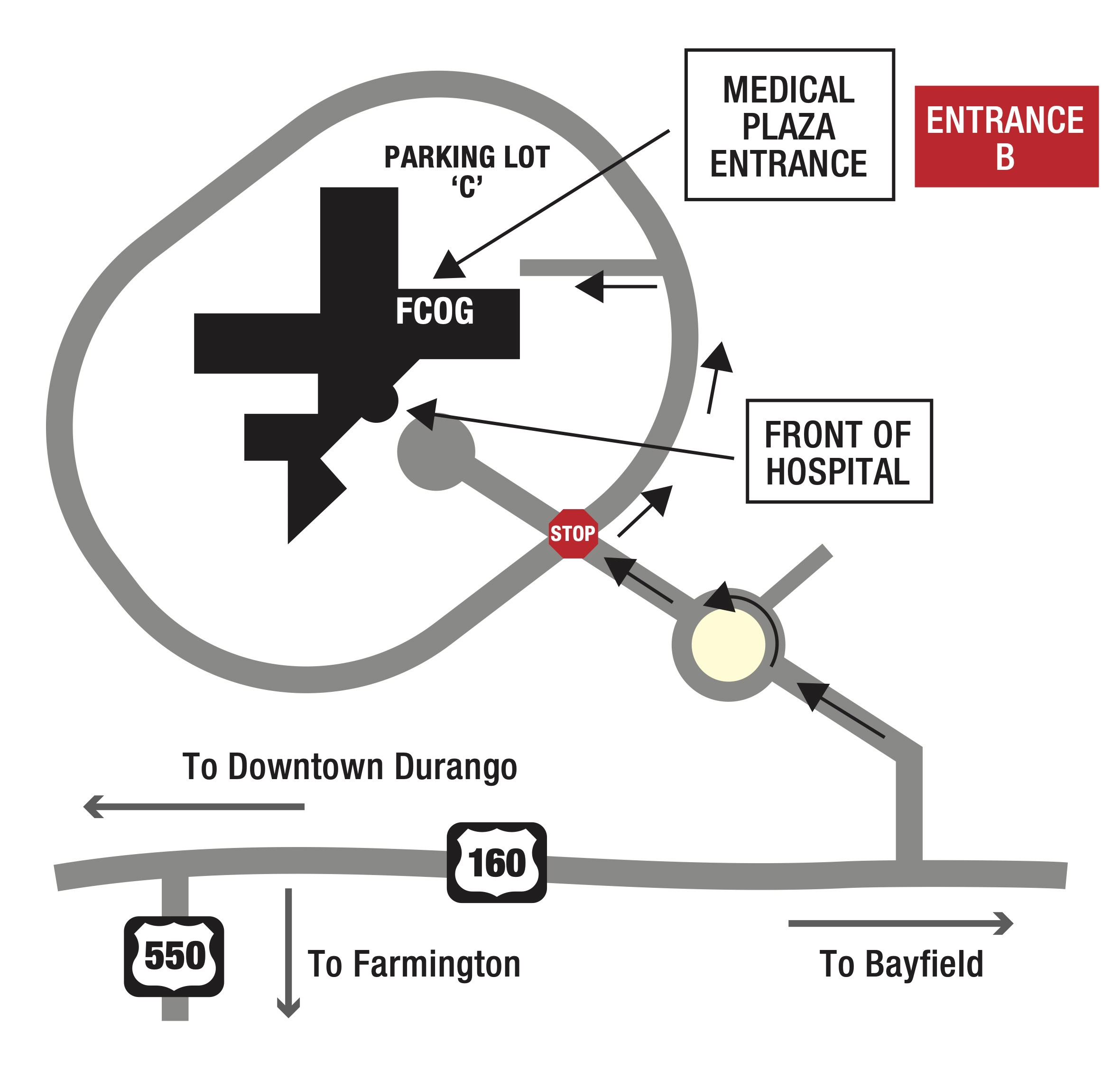
Our Location
Mercy Medical Plaza
1 Mercado Street, Suite 105
Durango, CO 81301
Open: Monday to Friday, 8:00a - 5:00p
Contact Numbers
Office: (970) 382-8800
Billing: (970) 852-0881
Fax: (970) 382-0122
Office Visit Protocol
If you are experiencing any fever or viral symptoms, please wear a mask over your nose and mouth.
If your child is sick, please avoid bringing them to the office, for the health and wellness considerations of other patients.
Patient Portal
Visit the patient portal and login to:
- Make online appointment requests
- Find online payment tools
- Access your healthcare information such as lab results
- Send a secure message to your physician and care team
Please allow 5 business days for response to messages through the Patient Portal. For quicker assistance, please call our office during business hours at (970) 382-8800.